-
-
Featured Care Areas

Cervical Cancer
What is cervical cancer?
Cervical cancer is an abnormal growth that forms in the cervix.
The cervix is part of the female reproductive system. It is a cylinder-shaped neck of tissue connecting the uterus and vagina, positioned at the lowermost portion of the uterus. The cervix produces cervical mucus that changes in consistency during the menstrual cycle to prevent or promote pregnancy.
In Singapore, cervical cancer is the 10th most commonly occurring cancer with the 8th highest cancer mortality rate.
99% of cervical cancer is caused by the human papilloma virus (HPV), which can be spread through sexual activity. HPV is a family of 100 over viruses, of which about 14 strains can cause cancer.
Types of cervical cancer
The 3 main types of cervical cancer are:
- Squamous cell carcinoma, which forms in the lining of the cervix. It is the most common type of cervical cancer, found in up to 90% of cases.
- Adenocarcinoma, which forms in the cells that produce mucus.
- Mixed carcinoma, which has features of both squamous cell carcinoma and adenocarcinoma.
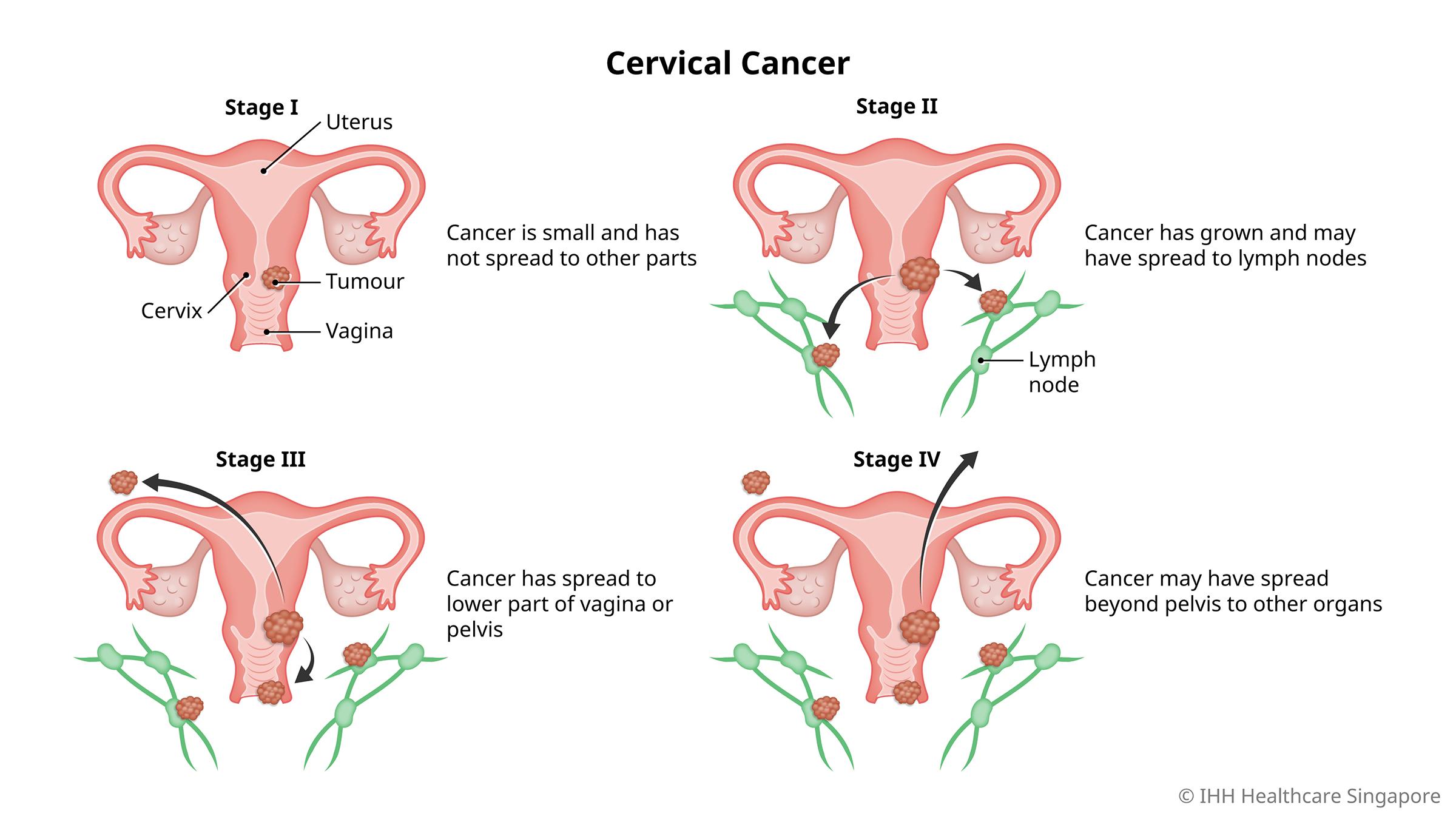
Stages of cervical cancer
Cervical cancer is assessed in 4 stages:
- Stage I: At this stage, the cancer is still small and has yet to spread to the lymph nodes or other parts of the body.
- Stage II: The cancer has grown larger and may have spread beyond the uterus and cervix, or to the lymph nodes.
- Stage III: The cancer has spread to the lower part of the vagina or the pelvis. It may have grown large enough to block the ureters (the tubes that carry urine from the kidneys to the bladder).
- Stage IV: The cancer may have spread further, beyond the pelvis and to organs such as the lungs, bone or liver.
What are the symptoms of cervical cancer?
Early stage cervical cancer may not present any symptoms.
However, you should see a doctor if you experience any of the following:
- Abnormal bleeding or discharge from the vagina
- Pain during sexual intercourse
- Lower back pain or pelvic pain
- Swollen legs
- Problems with urinating or defecating
What causes cervical cancer?
While the most common cause of cervical cancer is HPV, there are also genetic and lifestyle factors that may increase your risk.
What are the risk factors for cervical cancer?
- Sexual activity – Being sexually active from a young age and/or having multiple sexual partners increases the risk for cervical cancer.
- Family history of cervical cancer
- Smoking – This is a known carcinogen that increases the risk for many types of cancer, including cervical cancer.
- Oral contraceptives – These do not protect against sexually transmitted diseases like HPV. Use of oral contraceptives have also been linked to increased risk for cervical cancer.
What are the complications and related diseases of cervical cancer?
Complications of advanced cervical cancer include:
- Pain – This is a common symptom if the cancer has spread into nerve endings, bones or muscles.
- Kidney failure – In some cases, the tumour may lead to a build-up of fluid in the kidneys, which can lead to loss of kidney function.
- Blood clots – Tumours, especially large ones, may press on veins in the pelvic area, slowing the flow of blood to the legs. This can form a blood clot that causes pain, swelling or tenderness, warmth or redness in the legs. It can cause further complications or death if a clot travels to the lungs and blocks the flow of blood (pulmonary embolism).
- Bleeding – This can occur if the cancer spreads into the vagina, bowel, bladder or rectum.
- Fistula – This is a rare complication of advanced cervical cancer. A fistula is a channel that develops between the bladder and vagina, leading to persistent discharge of fluid from the vagina.
Complications arising from cervical cancer surgery include:
- Early menopause – Surgical removal of the ovaries or damage resulting from radiotherapy may trigger early menopause. This means your monthly periods will become irregular or cease and you may experience hot flushes, vaginal dryness, mood changes and other symptoms.
- Narrowing of the vagina – Radiotherapy may cause the vagina to narrow, which can make sexual intercourse painful or difficult.
- Lymphoedema – Removal of the lymph nodes in the pelvis may affect the lymphatic system’s ability to drain excess fluid. This can lead to a build-up of fluid in the tissues, known as lymphoedema, which can cause swelling. In cervical cancer, this usually affects the legs.
How do you prevent cervical cancer?
While there is no certain way to prevent cervical cancer, you can reduce your risk with the following ways:
- Cervical cancer screening – This is often known as a Pap smear, where cells are collected from the cervix and analysed for the presence of cancer cells. Another form of cervical screening is a HPV test which looks for the virus responsible for most cases of cervical cancer.
- HPV vaccination – This helps to protect against cancer-causing HPV strains. It is most effective when given before a person becomes sexually active. The vaccine can be given to both boys and girls.
- Limit exposure to HPV – Limit the number of sexual partners, and use a condom or other form of barrier protection during sexual intercourse.
- Quit smoking – You can reduce your risk for cervical cancer and other serious diseases by quitting smoking.
This page has been reviewed by our medical content reviewers.
Need help?
For enquiries, please call
+65 6575 7575
For appointment bookings, please WhatsApp
+65 8111 9777