-
-
Featured Care Areas

Take back control of your bladder health
Women are more prone to pelvic floor disorders than men due to their anatomical structure. For example, as many as 1 in 2 women will experience at least one urinary tract infection (UTI) during their lifetime.
Rather than suffer in silence, seek help from urogynaecologists, who specialise in the management and treatment of common women's conditions such as UTIs, incontinence or pelvic organ prolapse.
Contrary to popular belief, many of these conditions can be successfully resolved through a range of treatment options including changes in lifestyle and habits, non-invasive or minimally invasive procedures.
What is urogynaecology?
Urogynaecology is a subspecialty that combines urology and gynaecology to treat women with urinary tract disorders and pelvic floor dysfunction.
To diagnose and treat a urinary tract or pelvic floor disorder, a urogynaecologist will need to:
- Do a review of your medical history
- Perform a physical examination, such as a pelvic exam, or to check if there are any problems with your abdomen or kidneys
- Conduct certain tests, such as urine culture test for infection and urodynamic testing to look at how well parts of the lower urinary tract—the bladder, sphincters, and urethra—work to store and release urine
If you have a urogynaecological condition, it is vital to get yourself treated early as some of these conditions may lead to severe and life-threatening complications if left untreated. Early detection can also help prevent the need for surgery.
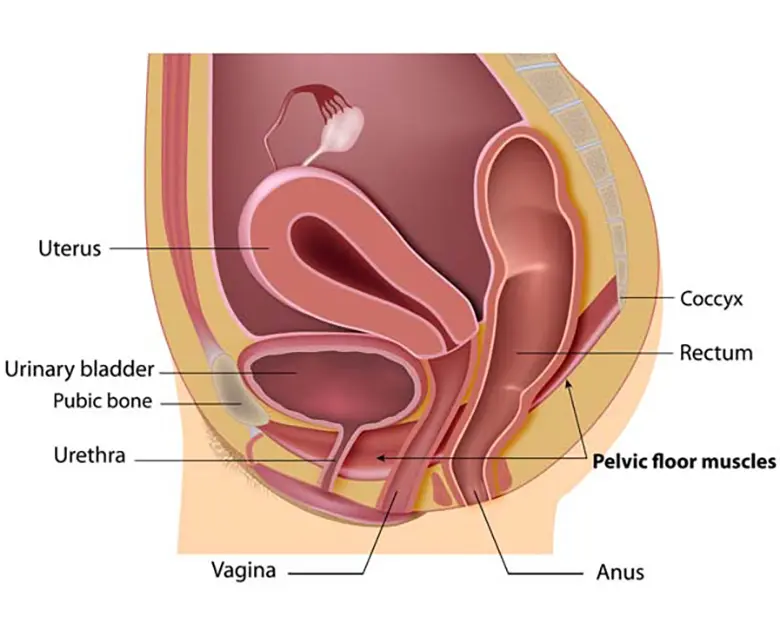
What is the pelvic floor?
The pelvic floor is the combination or muscles, connective tissue, ligaments and nerves that function to support and control the uterus, vagina, bladder, and rectum.
Occasionally, repeated heavy lifting, chronic disease, surgery, or childbirth may damage the pelvic floor. Pelvic floor dysfunction affects women of all ages, and encompasses a variety of conditions such as urinary tract infection, pelvic organ prolapse, or lower bowel problems.
Did you know? Twice as many women than men suffer from stress urinary incontinence. 1 in 3 are above 50 years old. As many as 80% of these women choose to suffer in silence and do not seek treatment.
Collapse All
What are the common pelvic floor and bladder conditions for women?
Common urogynaecological conditions affecting women include:
Urinary tract infections (UTIs) occur when the urinary tract becomes infected, usually caused by bacteria that enters the urinary tract via the urethra. They affect women more than men, with more than 50% of women experiencing at least one UTI in their lifetime.
UTIs are highly treatable with medication, but have a high recurrence rate. If left untreated, may lead to infection of the kidneys or even more severe health complications.
Urinary incontinence and voiding dysfunction occur when there is poor coordination between the bladder muscle and the urethra. As a result, activities such as laughing, coughing, or exercising may lead to urine leakage (urinary incontinence) or a complete loss of bladder control (voiding dysfunction).
Incontinence is a common problem and can develop at any age. The cause can be due to:
- Bladder hypersensitivity or urge incontinence
- Pelvic floor weakness or stress incontinence — this is more prevalent among older adults, especially in women who have given birth, undergone surgery or reached menopause
Tests can be done to differentiate these two causes as the treatment can differ. Medications can be used to treat bladder hypersensitivity while surgery is better for stress incontinence. Other interventions include laser therapy, lifestyle changes and physiotherapy.
Pelvic organ prolapse occurs when the pelvic organs drop from their original position in the pelvis. It is the result of weakened or damaged pelvic floor muscles which can no longer support the organs of the pelvis.
It is a common condition, especially among older women or women who have given birth, and can cause pain, discomfort and pressure in the vagina, as well as urinary and bowel problems.
Treatment depends on the type of prolapse, the woman's age, childbirth plans, as well as severity of the condition. It can consists of non-surgical treatment such as lifestyle changes and pelvic floor exercises, or surgery such as pelvic floor reconstruction.
This page has been reviewed by our medical content reviewers.