-
-
Featured Care Areas

Glomerulonephritis
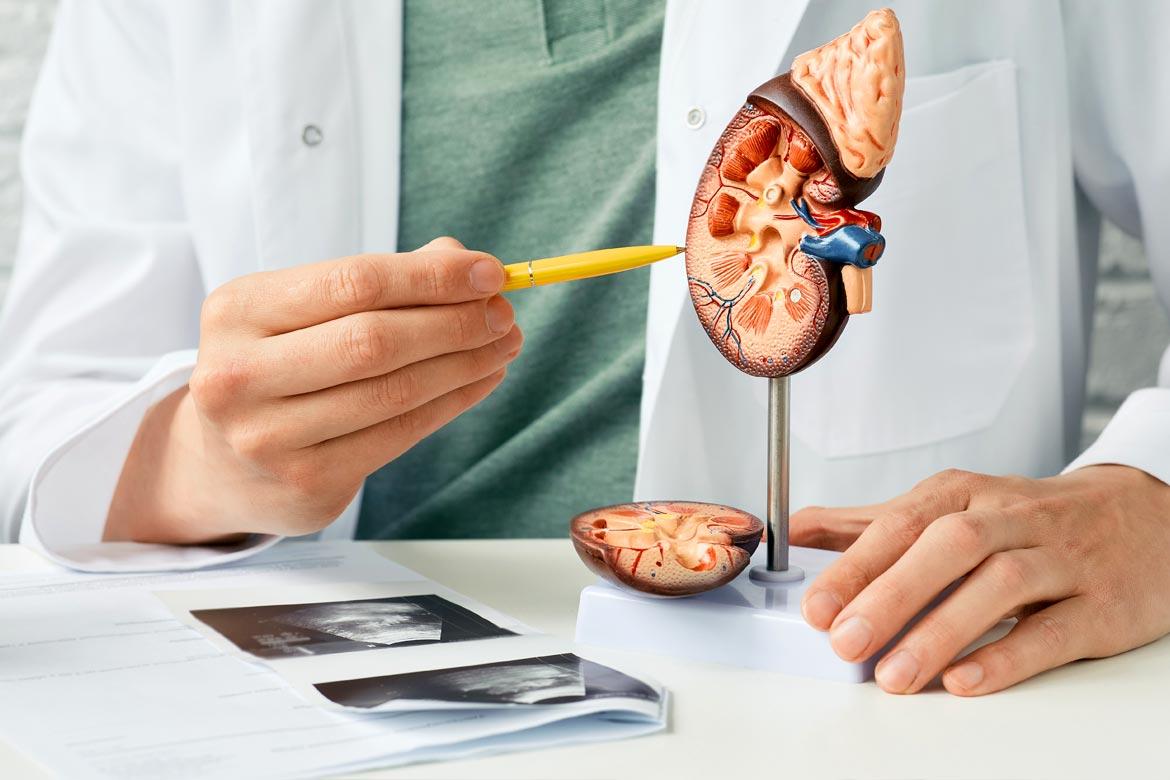
What is glomerulonephritis?
Glomerulonephritis is a kidney disease caused by the inflammation of small blood vessels in the kidney. The role of the glomeruli is to remove excess waste and fluid from your bloodstream and to excrete into your urine.
Glomerulonephritis due to either sudden onset of glomeruli inflammation (acute), or a gradual onset (chronic) causes the glomeruli to malfunction and the kidney to not be able to filter waste products from the blood normally.
There are 4 types of glomerulonephritis:
- IgA nephropathy. This is caused by the deposits of immunoglobulin A (IgA) in the glomeruli, which is characterised by occurrence of blood and protein in the urine. This disease can progress for years without noticeable symptoms.
- Focal segmental global sclerosis. This condition results from another disease or occurs without known reasons. It is characterised by scattered scarring of some of the glomeruli and can lead to kidney failure.
- Membranous glomerulonephritis. This condition occurs when the glomeruli become damaged and thickened. Protein leak results from the damaged blood vessels into the urine, which may cause signs and symptoms known as nephrotic syndrome.
- Systemic lupus erythematosus. This is a systemic autoimmune disease that occurs when the body's immune system attacks your tissues and organs. The inflammation caused by this condition can affect many different body systems, such as your joints, skin, kidneys, blood cells, brain, heart, and lungs.
What are the symptoms of glomerulonephritis?
The symptoms of glomerulonephritis are often experienced when the glomeruli are severely damaged. These include:
- Changes in urine colour (dark or pink)
- Foamy urine (due to protein in urine)
- Headache, sickness, fever and chills
- High blood pressure
- Reduced urine production
- Swelling of legs, hands and face due to excess fluid retention (oedema)
What are the causes of glomerulonephritis?
There are various conditions that can cause glomerulonephritis. These include:
- Autoimmune disease. Glomerulonephritis may be caused by a specific immune system problem (autoimmune disease). One such example would be IgA nephropathy, where antibody (immunoglobulin A) deposits in the glomeruli, causing the glomeruli to swell. The exact mechanism of IgA nephropathy is not fully understood, and the disease can develop for years before it is detected.
- Primary glomerulonephritis affects the kidneys directly
- Secondary glomerulonephritis is generally due to bacterial infections (streptococcal throat infection), viral infections (HIV and hepatitis viruses’ infections), heart infections (bacterial endocarditis), cancers, diabetes, high blood pressure and abscesses.
- Lupus. Inflammation caused by lupus can affect different areas of your body, including your kidneys. Lupus results in serious kidney damage. Kidney failure is one of the main causes of death among those with lupus.
- Goodpasture's disease. This rare immunological lung disorder can mimic pneumonia. Goodpasture's syndrome results in bleeding in the lungs, as well as glomerulonephritis.
What are the risk factors for glomerulonephritis?
Your chances of developing glomerulonephritis may increase with the following:
- Family history of kidney disease and infection. Genetic factors can play a role in glomerulonephritis.
- Immune system diseases. Conditions such as lupus and diabetes may cause scarring of the glomeruli that can also lead to glomerulonephritis. Protein in the urine and kidney failure might occur when growth factors activate the glomerular cells to produce scar materials.
- Long-term use of antibiotics or pain medications. Long-term use of certain medications that include non-steroidal anti-inflammatory drugs (NSAIDs), which are drugs that relieve or reduce pain, such as aspirin or ibuprofen, increase the risk of glomerulonephritis.
- Recent surgery of the urinary tract. Surgery can sometimes cause problems in your urine flow. Surgery complications may cause the urine to flow backward or reflux into your kidneys instead of flowing from your kidneys to your bladder.
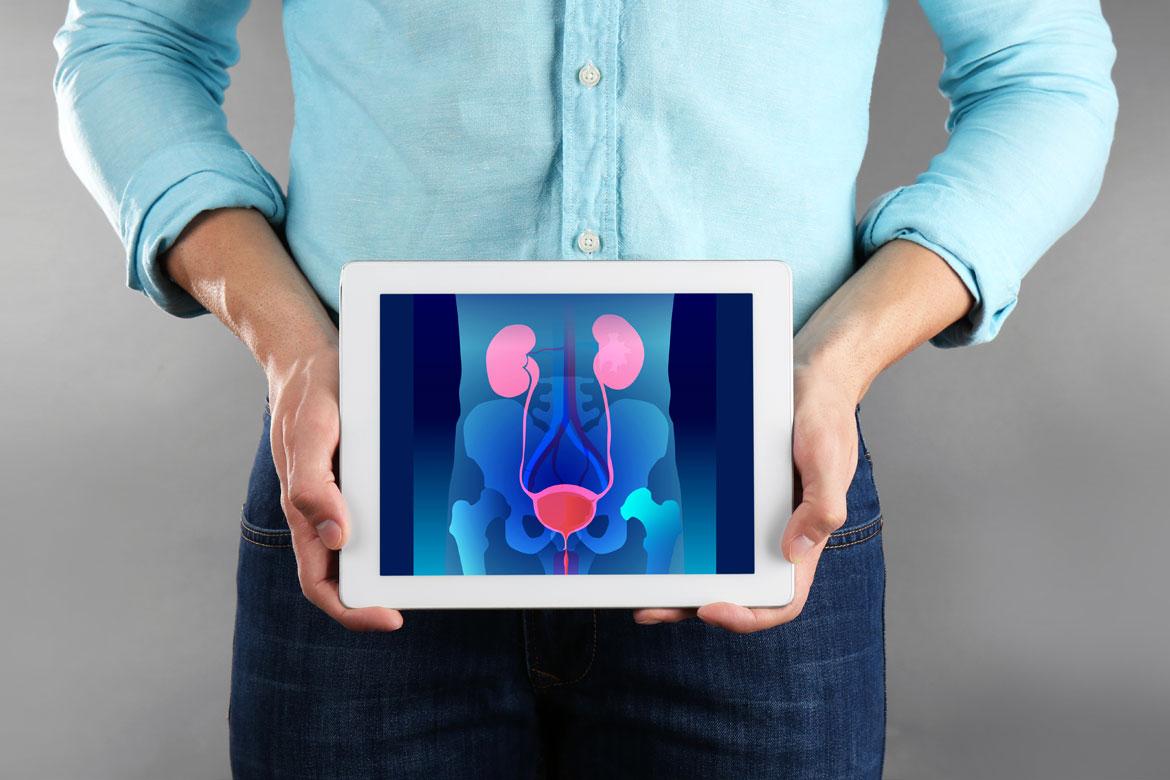
What are the complications and related diseases of glomerulonephritis?
Glomerulonephritis may lead to several health complications, including:
- High blood pressure. High blood pressure is a result of damage to your kidneys and the resulting build-up of wastes in the bloodstream. Blood pressure is indicated by the amount of blood your heart pumps and the amount of resistance to blood flow in your arteries.
- Kidney disease. Your kidneys may gradually lose their filtering ability. End-stage kidney disease that requires dialysis or a kidney transplant to sustain life may occur if kidney function deteriorates to less than 10% of normal capacity.
- Kidney failure. The deterioration of ability in the filtering part of the nephron results in the rapid accumulation of waste products. Emergency dialysis by an artificial kidney machine – an artificial means of removing extra fluids and waste from your body – will be necessary.
- Nephrotic syndrome. This syndrome occurs when there is too much protein in your urine that results in too little protein in your blood. It can be linked with high blood cholesterol and swelling or oedema of the feet, abdomen, and eyelids. Besides damaging the kidneys, such leakage of proteins may lead to increased risk of blood clots and elevated risk for some infections.
How do you prevent glomerulonephritis?
There is no way to prevent most forms of glomerulonephritis, but these steps can help lower your risk of developing the disease:
- Seek prompt treatment of a strep infection with a sore throat or impetigo
- Follow safe-sex guidelines and avoid intravenous drug use to prevent infections that lead to glomerulonephritis
- Prevent and control risk factors like hypertension, diabetes and obesity to minimise damage to the kidneys
This page has been reviewed by our medical content reviewers.
Need help?
For enquiries, please call
+65 6575 7575
For appointment bookings, please WhatsApp
+65 8111 9777