-
-
Featured Care Areas

Gastro-oesophageal Reflux Disease (GERD)
What is GERD?
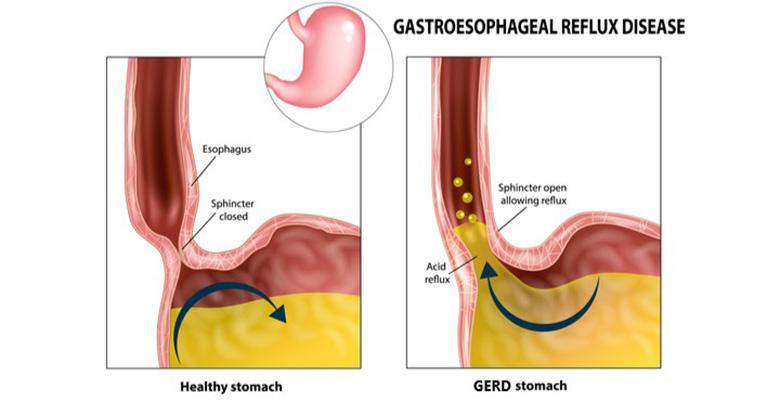
Gastroesophageal reflux disease (GERD), also known as acid reflux or heartburn, is a chronic digestive disease. It occurs when acid from the stomach flows back (reflux) into the oesophagus (food pipe). This acid reflux irritates, and can sometimes damage, the lining of the oesophagus. It can also reach the vocal cords or even flow back into the lungs.
In normal digestion, the muscular valve between the stomach and the oesophagus – known as the lower oesophageal sphincter – opens to allow food to pass into the stomach and closes to prevent food and acidic stomach juices from flowing back into the oesophagus. GERD usually occurs when the lower oesophageal sphincter is weak or faulty. This allows the stomach acid to flow back into the oesophagus.
Every once in a while, it is normal to experience acid reflux. However, if this occurs more than twice a week for a few weeks, it could be a sign of GERD.
What are the symptoms of GERD?
The most common symptom of GERD is heartburn, which is a burning sensation of the chest that spreads from the stomach to the throat. Other possible symptoms of GERD include:
- Burping
- Bloated stomach
- Hoarseness of voice
- Feeling of a lump in the throat
- Bitter taste in the mouth (acid regurgitation)
- Pain or discomfort in the chest
- Pain and difficulty swallowing
- Persistent sore throat
- Persistent cough
What causes GERD?
There is no identifiable sole cause of gastroesophageal reflux disease. GERD usually occurs when the muscular valve between the stomach and the oesophagus is weak or faulty. This allows the stomach acid to flow back into the oesophagus.
What are the risk factors for GERD?
The following factors can lead to the onset of GERD or aggravate acid reflux:
- Certain diseases, such as Zollinger-Ellison syndrome or scleroderma.
- Increased abdominal pressure due to obesity or pregnancy.
- Increased production of gastrin, a hormone that regulates the release of stomach acid.
- Hiatal hernia, a condition where the upper part of the stomach moves up into the chest through an opening in the diaphragm. This condition lowers the pressure in the oesophageal sphincter.
- Certain medications, including asthma medicine, calcium channel blockers, antihistamines, painkillers, sedatives, and antidepressants.
- Certain foods and beverages, such as fried, spicy, or fatty foods, chocolate, peppermint, coffee, or alcoholic beverages.
- Smoking or inhaling second-hand smoke.
What are the complications and related diseases of GERD?
GERD can sometimes lead to the following complications:
- Swelling of the vocal cords, also known as reflux laryngitis
- Stricture (blockage) of the oesophagus, caused by scar tissues that develop due to repeated ulcerations
- Barrett’s oesophagus, a change in the oesophagus tissue caused by long-lasting GERD which increases the risk of esophageal cancer
- Lung damage which may include pulmonary fibrosis and bronchiectasis
- Ulcers in the oesophagus, caused by burning from stomach acid
How to prevent GERD?
Several lifestyle changes and over-the-counter medications can be taken to control gastroesophageal reflux. These can also help prevent or reduce the risk of the condition turning into a chronic disease.
To control GERD, you should:
- Avoid overeating
- Avoid eating 2 – 3 hours before bedtime
- Avoid trigger food and beverages, such as fried, spicy, or fatty foods, chocolate, peppermint, coffee, or alcoholic beverages
- Lose weight if you are overweight or obese
You may also consider the following over-the-counter medicine:
- Antacids for mild GERD
- H-2-receptor blockers or certain proton pump inhibitors for chronic or moderate GERD
This page has been reviewed by our medical content reviewers.
Need help?
For enquiries, please call
+65 6575 7575
For appointment bookings, please WhatsApp
+65 8111 9777