-
-
Featured Care Areas

Uterine Fibroid (Myoma)
What are uterine fibroids?
A uterine fibroid is a non-cancerous growth in the uterus (womb). It can grow on the inside of the uterus, within the muscle wall of the uterus or on the outer surface of the uterus. Uterine fibroids are also known as myomas.
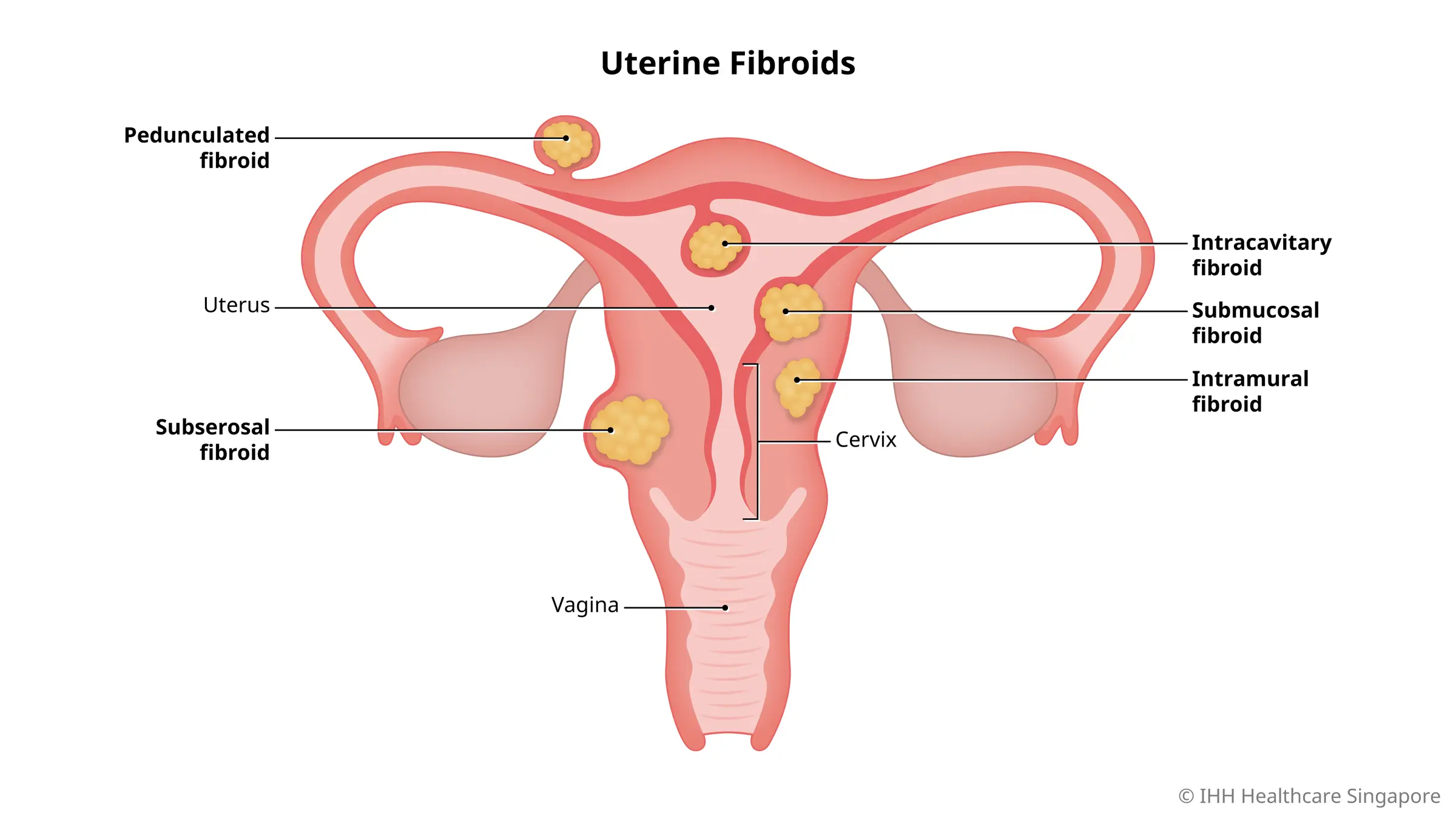
Types of uterine fibroids
Uterine fibroids are classified according to their location in the uterus.
- Intracavitary. This type of uterine fibroid is almost completely within the womb cavity. It extends into the uterine cavity.
- Intramural or intramyommetrial. This is the most common type of uterine fibroid. It is located completely within the womb muscle.
- Pedunculated. Pedunculated fibroids are located on the outer and inner wall of the womb. They are attached to the womb surface by a stalk. When sudden movements cause these fibroids to rotate, you may feel sudden and intense pain.
- Submucous. This type of uterine fibroid is located partially in the womb cavity, starting from its wall. This is the least common type of uterine fibroid. It can cause heavy bleeding and is most closely related to a fertility problem.
- Subserous. Subserosal uterine fibroids protrude outside the womb, with the base on the outer surface of the womb. These fibroids may cause pressure, but they do not usually cause bleeding.
How do uterine fibroids grow?
Uterine fibroids have different growth patterns. Some grow slowly, while others grow rapidly. Some do not grow in size at all, while some uterine fibroids go through growth spurts.
There are also uterine fibroids that resolve on their own. For example, fibroids that developed during pregnancy may shrink or completely disappear as the uterus returns to its normal size after pregnancy.
What are the symptoms of uterine fibroids?
Your symptoms depend on the location and size of the uterine fibroids. Common symptoms include:
- A sense of pressure or discomfort in the lower abdomen (belly) or pelvis.
- Abdominal pain. The pain may be acute or chronic, but persistent and localised.
- Constant back pain, due to a fibroid pressing against the muscles and nerves of your lower back.
- Difficulty passing stools, as rectal pressure from a fibroid can cause a feeling of fullness.
- Discomfort or pain during sexual intercourse. Inform your doctor if you experience this.
- Vaginal bleeding, passing of blood clots or prolonged menstrual periods.
- The need to urinate frequently or inability to urinate despite a full bladder.
Seek urgent medical attention if you have severe fibroid symptoms such as:
- Excessive vaginal bleeding
- Sudden, sharp pelvic pain
- Pelvic pain that does not go away
- Prolonged or painful heavy menstrual periods
- Bleeding or spotting between periods
- Difficulty emptying your bladder
- Unexplained low red blood cell count
What causes uterine fibroids?
The causes of uterine fibroids remains unclear, but may be linked to these factors:
- Genetic factors. There may be a hereditary link to close family members with the condition.
- Hormones. Oestrogen and progesterone, the sex hormones, may promote the growth of a fibroid. These fibroids often shrink after menopause as the body produces less oestrogen and progesterone.
- Other growth factors. These include substances that help the body maintain tissues, e.g. insulin-like growth factor.
What are the risk factors for uterine fibroids?
These factors may increase your risk of developing uterine fibroids:
- Age. Women of reproductive age are at higher risk.
- Family history. If family members have a history of having fibroids, you may have a higher risk.
- Obesity
- Early onset of menstruation
- Vitamin D deficiency
- Diet higher in red meat
- Diet that is low in dairy, green vegetables and fruits
- Alcohol consumption
What are the complications and related diseases of uterine fibroids?
Although uterine fibroids are not usually dangerous, they can cause discomfort and may lead to complications of anaemia (low red blood cell count) from heavy blood loss. Learn more about growths such as fibroids, polyps, and ovarian cysts, and get a more in-depth look at uterine fibroids and their associated potential complications.
How do uterine fibroids affect pregnancy?
Uterine fibroids can occasionally cause infertility or miscarriage, or prevent implantation and growth of an embryo. Rarely, uterine fibroids can block your fallopian tubes or affect the passage of sperm from your cervix to your fallopian tubes.
How do you prevent uterine fibroids?
Though there is no proven way to prevent uterine fibroids, adopting a healthy lifestyle may lower your risk. These include maintaining a healthy weight and eating more fruits and vegetables.
This page has been reviewed by our medical content reviewers.
Need help?
For enquiries, please call
+65 6575 7575
For appointment bookings, please WhatsApp
+65 8111 9777