Edwin Chng Aik Chen
General Practitioner

Source: Getty Images
General Practitioner
The World Health Organization (WHO) first rang the alert about the spread of monkeypox, a rare infectious disease, in May 2022. Since then, increasing cases of monkeypox infections have been reported in non-endemic countries after being first detected in Europe. At the time of publication, the latest WHO statement points to over 7,000 reported monkeypox infections across 60 countries with 1 death confirmed. The virus has also made its way to Singapore, with 3 cases (1 local infection, 2 imported) as of 7 July 2022.
Dr Edwin Chng, medical director at Parkway Shenton, shares more about the virus, its means of transmission, and the symptoms that may be experienced in a monkeypox infection.
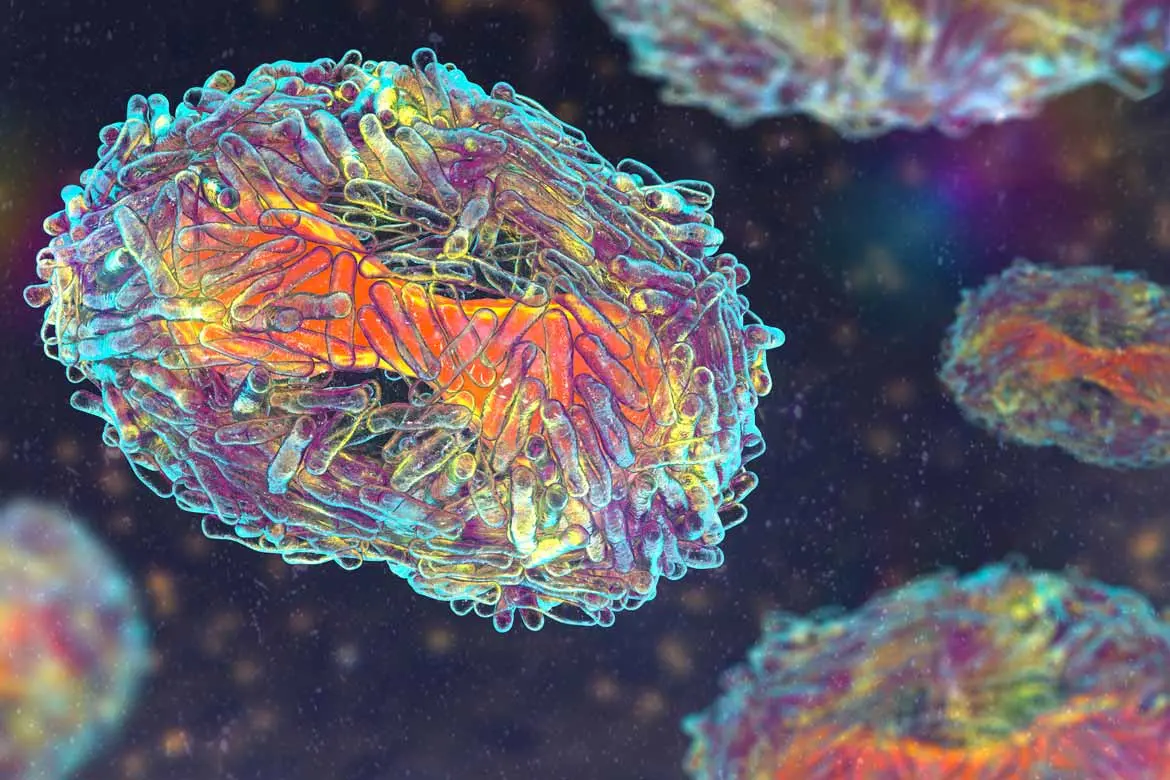
Monkeypox is a rare disease caused by infection with the monkeypox virus, which is of the same genus as the smallpox virus. There are two distinct strains of monkeypox: a strain from West Africa and a strain from Central Africa, with the former being less virulent. The strain involved in the current worldwide outbreak in non-endemic countries appears to be from West Africa.
The source of the disease remains unknown, but it is named monkeypox because it was first discovered in Denmark in 1958. The virus had been isolated from a colony of laboratory monkeys from Singapore that were going to be used for polio virus research.
The first human case was later recorded in 1970 in the Democratic Republic of the Congo. Since then, other cases have surfaced in Central and West Africa. There were also sporadic cases outside Africa due to international travel or through imported animals.
Transmission of monkeypox can occur in two ways:
This occurs through contact with an infected animal’s bodily fluids or through a bite. Animals known to carry the monkeypox virus or have monkeypox infections include monkeys, squirrels, rats, and dormice. The type of exposure can affect a person’s risk of infection and severity of disease.
For example, patients who were bitten or scratched are more likely to develop more severe disease compared to those who had contact by touching an infected animal.
This occurs mainly through direct contact with sores, scabs or bodily fluids.
In this present outbreak, close contact with skin lesions during sexual activities is considered the main risk factor. Indirect transmission can occur through contact with contaminated materials (fomites) such as clothing and bed linen. The virus may also be spread though respiratory secretions during prolonged face-to-face contact. It is not known if the virus can spread though semen or vaginal fluids, but it can be passed from a mother to her foetus (by crossing the placenta), resulting in congenital infections.
The incubation period of the monkeypox virus ranges between 4 – 21 days. Early symptoms of an infection include fever, chills, body aches, headache, enlarged lymph nodes and fatigue. This typically lasts up to 5 days.
The characteristic painful rash typically starts within 1 – 4 days after the onset of fever, and can remain for up to 3 weeks. The rash is usually concentrated on the face, palms and soles of the feet, but can involve the patient’s genitals, rectum, eyes and mouth as well.
A monkeypox infection is self-limiting in most patients, and they usually recover in 2 – 4 weeks. Treatment is typically supportive (to relieve symptoms), and antiviral drugs are typically only started on patients with severe disease, or at risk of severe disease. Complications of monkeypox infections do occur, and they include bacterial infections of the rash, pneumonia, infection of the brain, and blindness.
A patient is considered to be infectious from the onset of illness till all the scabs from the lesions have fallen off and re-epithelialisation has occurred (when the areas of the skin turn a light pink with a shiny pearl appearance). Hence, it is important to quickly identify and isolate infected patients to prevent spread of the virus to others.
Any one who has been exposed to an infected person with monkeypox, or is at risk of infection, should monitor themselves for symptoms over a period of at least 21 days after the last exposure. Contacts who remain asymptomatic can continue routine daily activities, but they must immediately self-isolate and seek medical help if any symptoms develop.