-
-
Featured Care Areas

Minimally Invasive Cardiac Surgery
What is minimally invasive cardiac surgery?
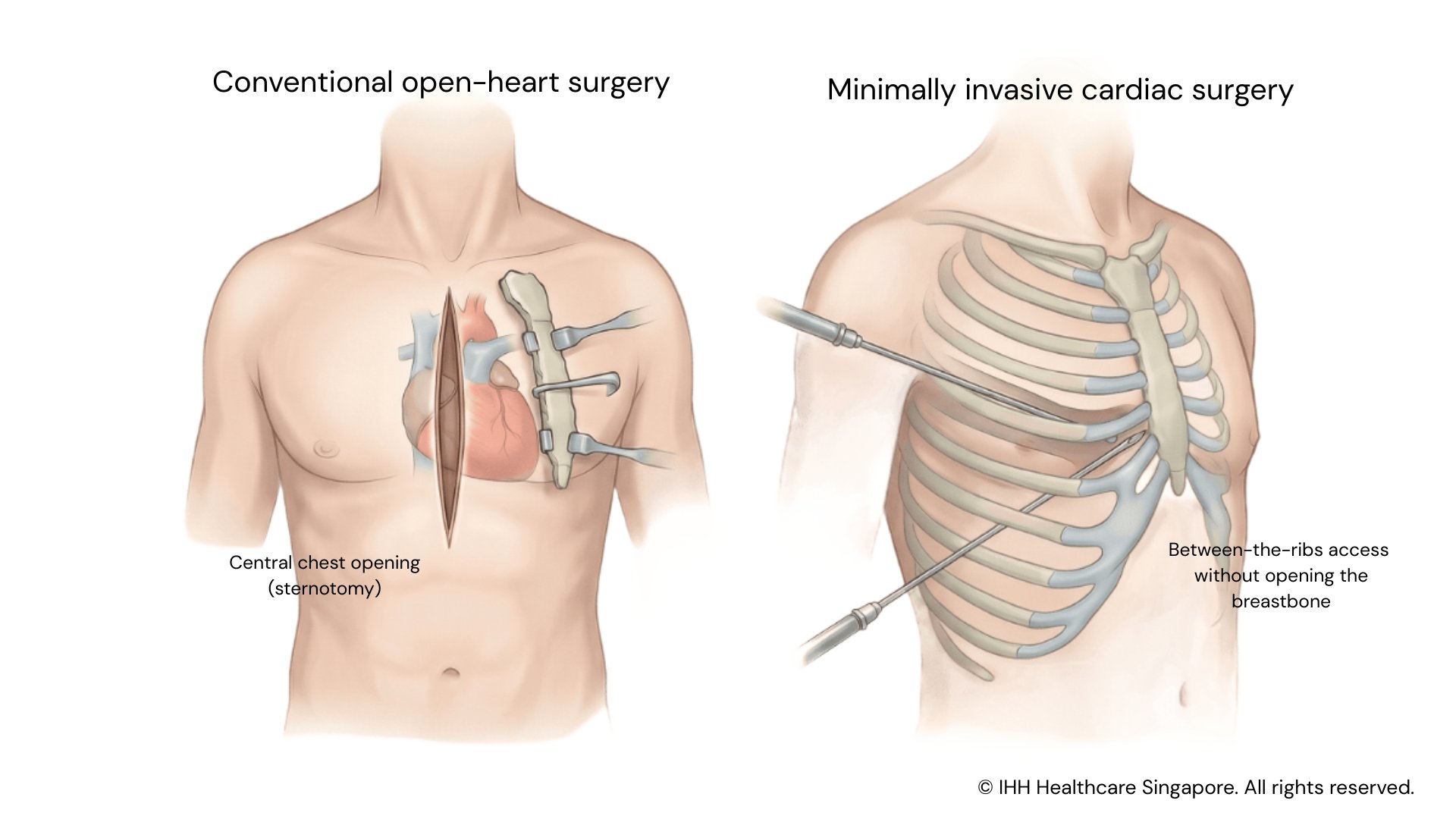
Minimally invasive cardiac surgery (MICS) refers to a group of heart operations performed through small incisions in the chest, rather than opening the breastbone (sternotomy) as in traditional open-heart surgery.
Sometimes described as keyhole heart surgery or small-incision heart surgery, MICS allows surgeons to treat certain heart conditions while reducing trauma to the chest wall.
MICS achieves the same surgical objectives as conventional open-heart surgery, but with potential benefits such as less pain, smaller scars, shorter hospital stays and faster recovery, where clinically appropriate.
How it works
In minimally invasive cardiac surgery, surgeons access the heart through small incisions between the ribs, instead of cutting through the breastbone. Specialised surgical instruments and camera guidance are used to visualise and operate on the heart.
Depending on the type of procedure, the heart-lung bypass machine may still be used, even though the chest is not fully opened. The exact approach depends on the heart condition being treated, the patient’s anatomy, and the complexity of surgery.
Minimally invasive cardiac surgery vs open-heart surgery
Both minimally invasive and traditional open-heart surgery aim to correct the same underlying heart conditions. The main difference lies in how the heart is accessed.
Compared with open-heart surgery, minimally invasive cardiac surgery is performed through smaller chest incisions, avoiding the need to open the breastbone. This approach may offer several advantages, including:
- Faster recovery, with most patients able to resume usual daily activities within 2 – 4 weeks
- Less postoperative pain and scarring
- Reduced physical and psychological trauma associated with surgery
- Shorter hospital stay, with earlier discharge typically within 3 – 4 days
- Better early lung function after surgery
- Lower risk of infection and bleeding
In some cases, open-heart surgery may still be the safest or most effective option for patients with complex or extensive heart conditions. The most appropriate surgical approach will be carefully assessed and recommended by your surgeon based on your individual condition and overall health.
Why do you need minimally invasive cardiac surgery?
Minimally invasive cardiac surgery may be recommended to treat certain heart conditions that require surgical correction, including:
- Heart valve diseases such as mitral or aortic valve disorders
- Coronary artery disease requiring bypass surgery
- Congenital heart defects such as atrial septal defects (ASD) and ventricular septal defects (VSD)
- Selected heart rhythm conditions requiring surgical intervention
MICS may be considered when catheter-based treatments are not suitable, or when minimally invasive surgery offers better long-term outcomes. The decision to proceed with minimally invasive surgery depends on your condition, anatomy, overall health and surgical complexity.
What are the types of minimally invasive cardiac surgery?
At our hospitals, MICS may be used to treat selected heart conditions using small chest incisions instead of opening the breastbone. The specific approach depends on the condition being treated, anatomical considerations, and overall suitability for minimally invasive techniques. Types include:
Minimally invasive mitral valve repair or replacement
Minimally invasive mitral valve surgery is commonly performed to treat mitral regurgitation (leakage of the valve) or mitral stenosis (narrowing of the valve). Through a small incision on the side of the chest (mini-thoracotomy), surgeons can access the mitral valve without opening the breastbone.
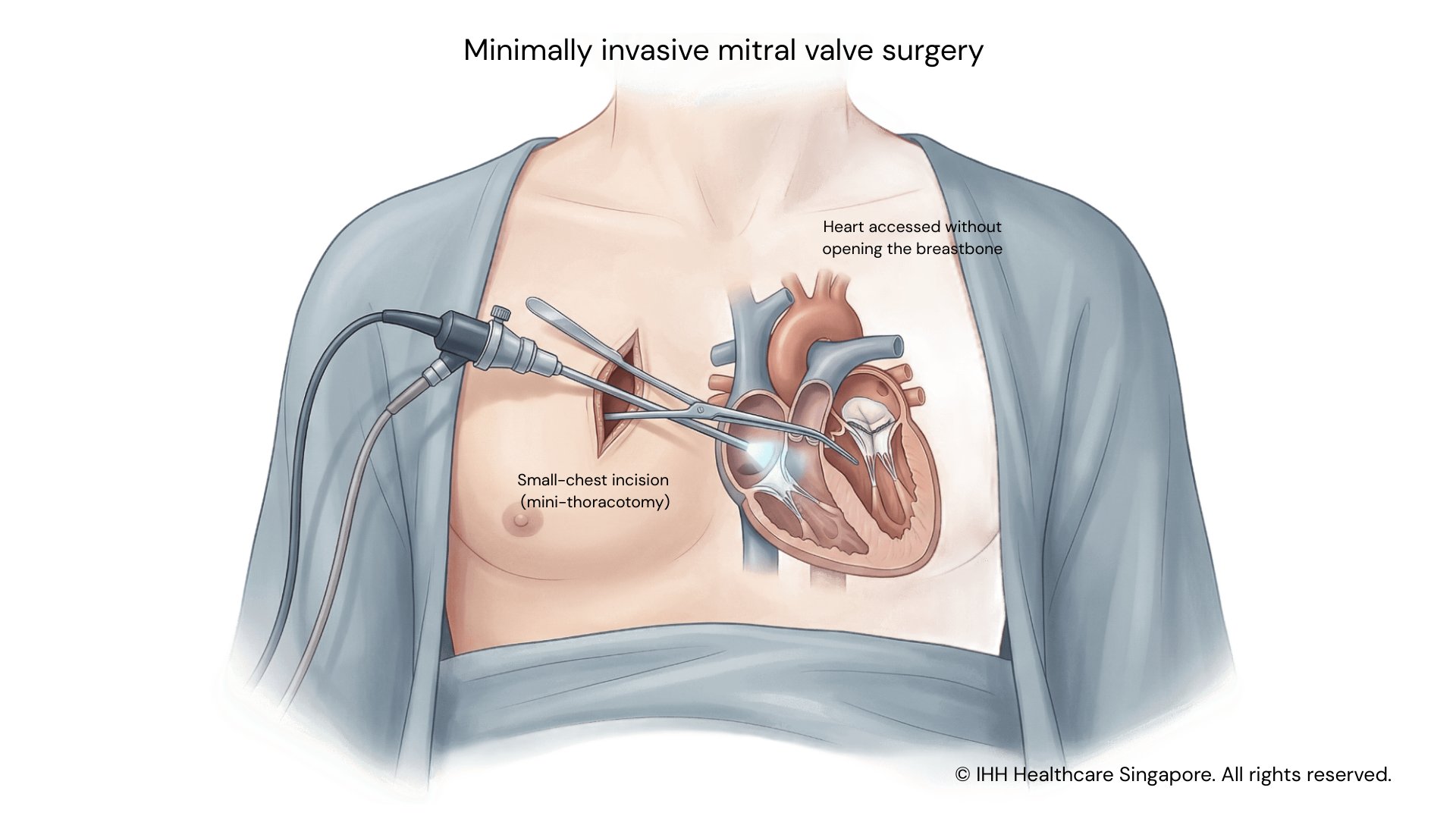
Depending on the condition of the valve, the procedure may involve repairing the native valve or replacing it with a prosthetic valve. Camera-assisted (endoscopic) techniques are often used to enhance visualisation during surgery.
Compared with open-heart surgery, this approach may result in less pain, smaller scars and faster recovery in suitable patients.
Minimally invasive aortic valve replacement
Minimally invasive aortic valve replacement is used to treat aortic valve narrowing (aortic stenosis) or aortic valve leakage (aortic regurgitation) when surgical intervention is required.
In qualifying patients, the valve can be replaced through a small incision on the chest, sometimes with the aid of a specialised camera, avoiding a full sternotomy. This surgical approach aims to relieve symptoms, improve blood flow from the heart, and preserve heart muscle function, while offering the potential benefits of reduced surgical trauma and earlier recovery.
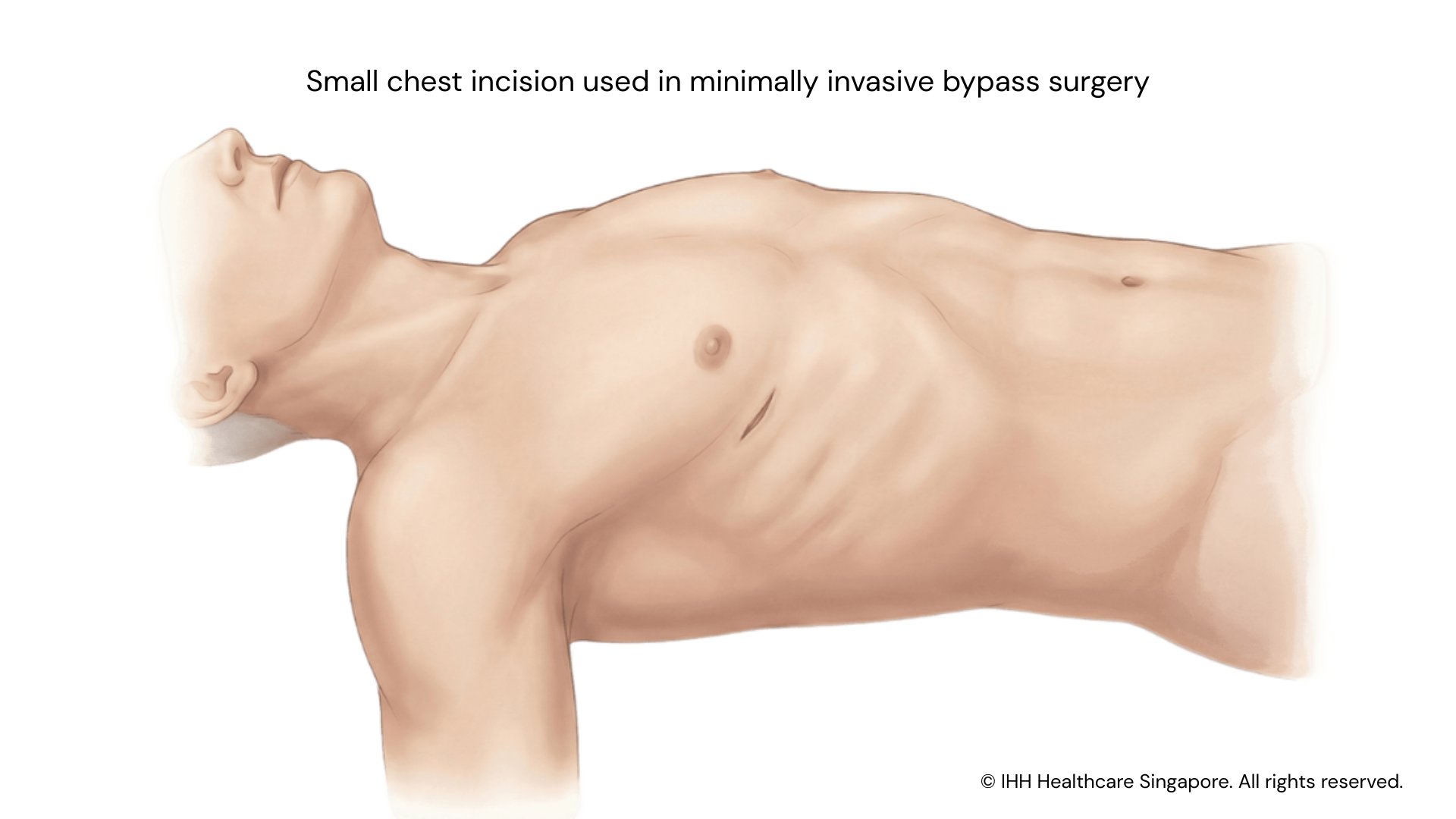
Minimally invasive coronary artery bypass surgery
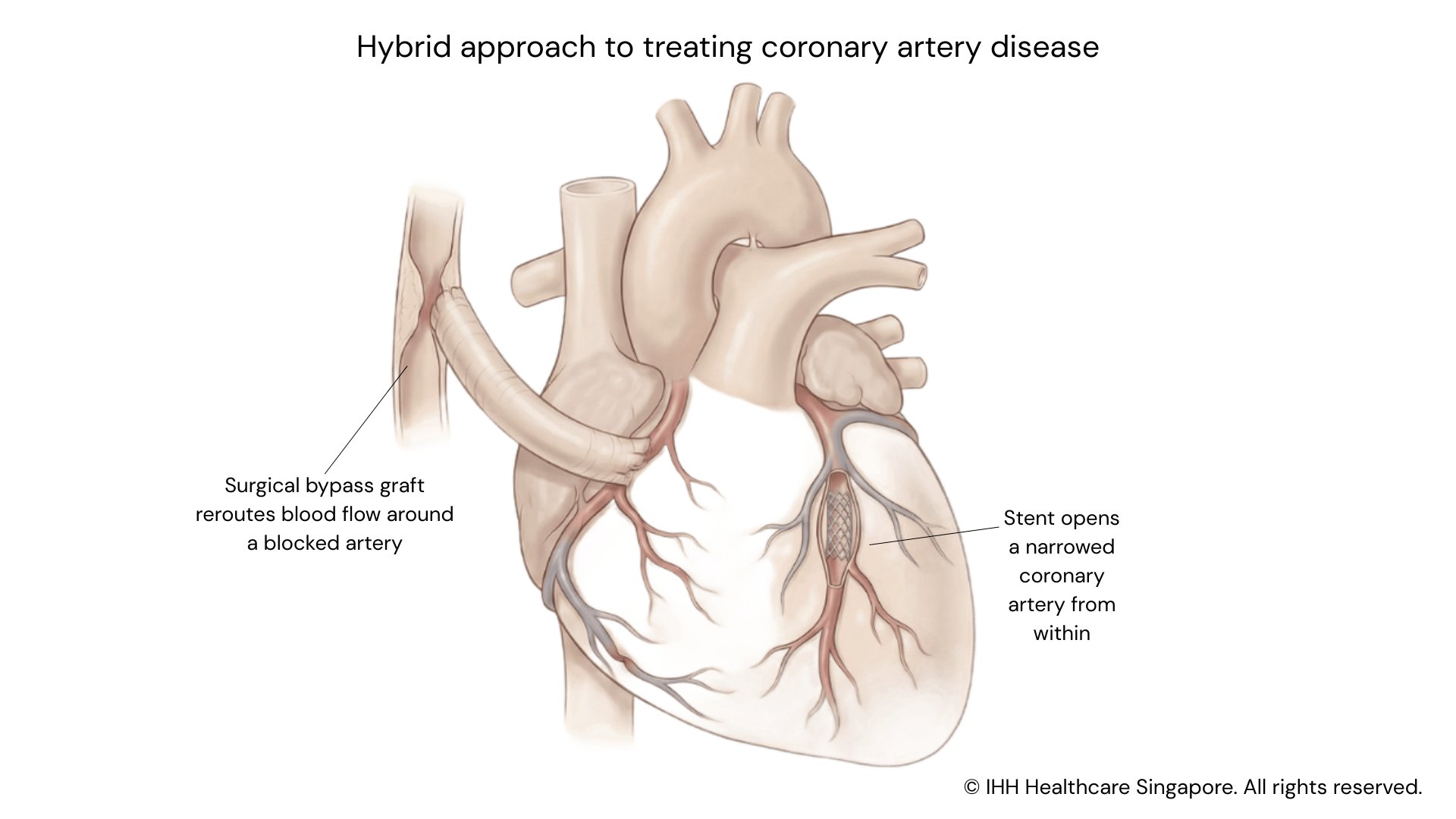
Minimally invasive coronary artery bypass surgery (CABG) may be used to treat coronary artery disease in selected patients, including those requiring single- or multi-vessel grafting.
Through a small incision on the side of the chest, surgeons can bypass blocked coronary arteries to restore blood flow to the heart muscle without opening the breastbone.
In some cases, this may form part of a hybrid approach, where bypass surgery is combined with stent placement (angioplasty) to treat other narrowed arteries. This allows patients to benefit from both surgical and catheter-based techniques, where clinically appropriate.
Minimally invasive repair of congenital heart defects (ASD and VSD)
Certain congenital heart defects, such as atrial septal defects (ASD) and ventricular septal defects (VSD), can be repaired using minimally invasive surgical techniques.
These procedures are performed through small incisions on the side of the chest, avoiding the need for a traditional sternal split. Minimally invasive repair allows surgeons to correct abnormal blood flow between heart chambers while potentially reducing recovery time and postoperative discomfort.
Minimally invasive removal of heart tumours
Selected heart tumours, such as atrial myxomas, fibroelastomas, and other benign growths within the heart, can be removed using minimally invasive techniques.
Through a small chest incision, with or without camera assistance, surgeons can safely access and remove these tumours. This approach allows for effective treatment while minimising surgical trauma and supporting a smoother recovery.
Minimally invasive surgery for selected redo cases
In certain patients who have undergone previous heart surgery, repeat (redo) procedures may still be possible using a minimally invasive approach.
By avoiding reopening the breastbone, minimally invasive techniques may reduce surgical risk in carefully selected redo cases. Suitability depends on multiple factors, including the type of previous surgery, scar tissue, and the current heart condition.
In selected patients, minimally invasive techniques may also be applied to other valve, bypass, congenital or rhythm-related heart conditions, depending on clinical suitability and surgical assessment. Not all minimally invasive approaches are appropriate for every patient, and the most suitable technique will be advised by the treating surgeon.
When open-heart surgery isn't the only option
Who should not undergo minimally invasive cardiac surgery?
Most patients assessed in Mount Elizabeth’s heart programme are considered suitable candidates for minimally invasive heart surgery.
Drawing on the expertise of Prof Theodoros Kofidis and our broader team of cardiac specialists, we offer a wide range of procedures across the heart-surgery spectrum with proven outcomes.
Some patients may not be suitable for minimally invasive or endoscopic approaches due to anatomical or clinical considerations. In selected cases, certain procedures can also be performed on a beating heart, depending on what is safest and most appropriate for the individual.
To determine whether you are a candidate for minimally invasive heart surgery, your doctor is likely to:
- Review your medical history
- Conduct a physical examination
- Perform tests (such as imaging tests, laboratory tests, pulmonary function tests and cardiac evaluation)
Your doctor and treatment team will work with you to determine the best option to treat your condition.
What are the risks and complications of minimally invasive cardiac surgery?
As with all heart surgeries, minimally invasive cardiac surgery may carry potential risks and complications, which vary depending on the procedure and individual health factors. These may include:
- Bleeding
- Infection
- Irregular heart rhythms (arrhythmias)
However, minimally invasive heart surgery generally carries advantages over open-heart surgery. These include:
- Less risk for bleeding
- Less risk for infection
- Less risk for irregular heart rhythms (arrhythmias)*
- Same risk for stroke
- Same risk for death
If your surgeon thinks it is not safe to continue with the minimally invasive heart surgery approach, your procedure may need to be changed to open-heart surgery.
Why choose Gleneagles Hospital?
At Gleneagles Hospital, our team of cardiologists and cardiothoracic surgeons are known in Singapore and the region for their expertise in treating complex heart conditions.
Our cardiovascular team offers a range of sophisticated treatment options and surgical procedures such as minimally invasive heart surgery and video-assisted thoracoscopic surgery (VATS).
Find doctors from our allied hospitals
We offer a full spectrum of healthcare services under IHH Healthcare Singapore.
Check if your preferred hospital offers this treatment:
This page has been reviewed by our medical content reviewers.
Need help?
For enquiries, please call
+65 6575 7575
For appointment bookings, please WhatsApp
+65 8111 9777