-
-
Featured Care Areas


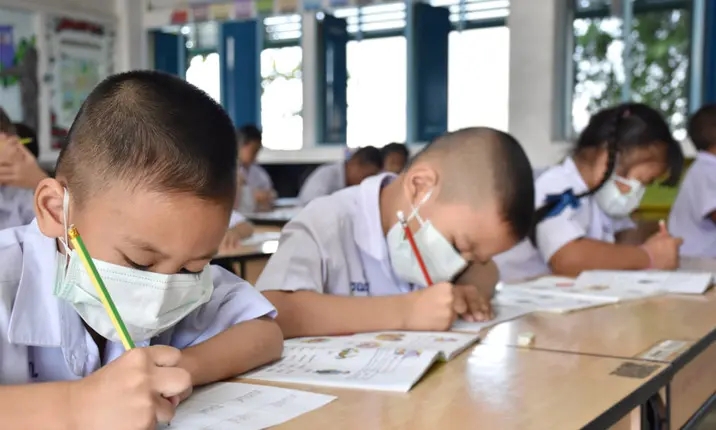
Source: Shutterstock
COVID-19 and Children: 12 Things to Know
Last updated: Wednesday, February 9, 2022 | 12 min reading time
How does COVID-19 impact our little ones and what can we do to care for them and keep them safe?
Singapore is dealing with a wave of infections from the highly transmissible Omicron variant of COVID-19. While vaccinations have proved effective in limiting the incidence of serious illness, children under the age of 12 have been increasingly making up hospitalisation numbers, with some 14,380 children under 12 years old infected with COVID-19 between October 2021 and January 2022.
Naturally, as a parent, you might be worried, especially about the risks of catching COVID-19, its effects on your child, concerns about vaccination, and how to care for your child should they get infected by the virus.
Dr Mohana Rajakulendran, paediatrician and mother of two, provides evidence-backed answers to 12 practical questions parents and caregivers might have about COVID-19.
Q1: Why are more children being sent to hospital for COVID-19?
Infants under the age of 1 have a slightly higher risk of having more severe COVID-19 symptoms. This is why they will be monitored more closely. Children who have underlying medical conditions such as congenital heart disease, neurological or metabolic disorders, certain genetic conditions, obesity or asthma may also be at higher risk of more severe symptoms and require closer observation.
As with any viral illness, some children may need to undergo investigations for prolonged fevers, or unusually high temperatures. They may also require fluid support for symptoms such as poor appetite, vomiting and diarrhoea, as this may lead to dehydration. Children who develop respiratory issues with shortness of breath, or low oxygen levels, may require oxygen support.
Q2: How serious are the health risks to my child if they catch COVID-19?
While many of the children who develop COVID-19 infections may be asymptomatic, or experience mild symptoms such as fever, cough, diarrhoea or fatigue, a small number of them may develop complications.
Amongst the 14,380 children under 12 years old infected with COVID-19 in Singapore from October 2021 to January 2022, 15 developed Multisystem Inflammatory Syndrome in Children (MIS-C), or at an incidence rate of 0.1%. MIS-C is an inflammatory syndrome that may develop 2 – 6 weeks after the initial COVID-19 infection, affecting multiple organ systems such as the heart, kidneys, lungs, intestines, brain and bone marrow. These children usually present symptoms such as prolonged high fevers, rashes, red eyes and lips, swollen lymph nodes, dizziness, stomach pains, vomiting and diarrhoea. Some may have poor heart function and low blood pressure, requiring support in the Intensive Care Unit.
With regard to the incidence of long COVID-19 in children, a study conducted in Rome from March 2020 to October 2020 has shown that up to 42.6% of children continue suffering from symptoms such as fatigue, muscle aches, headaches, insomnia, respiratory issues or palpitations for months after recovery from the initial COVID-19 infection.
More recently, Yale Medicine has reported that their doctors are treating children with long COVID-19 who face joint pain, fatigue and brain fog amongst other symptoms. These symptoms are presenting themselves in different intensities and durations, and in some cases last for months. While doctors have made progress in learning about the causes of long COVID-19 in children and the solutions, research is underway to learn more. Challenges include tracking the incidence of long COVID-19 in children, as young children may have trouble verbalising the symptoms they face, leading to it falling under the radar.
Q3: What are the symptoms of COVID-19 in children?
Children with COVID-19 may experience any of the following symptoms 2 – 14 days after exposure:
- Fever
- Cough
- Sore throat
- Shortness of breath
- Runny nose
- Sneezing
- Loss of sense of smell or taste
- Gastrointestinal symptoms like diarrhoea or vomiting
They may also be asymptomatic but still be infected with COVID-19.
Q4: How should I seek medical help if I think my child has COVID-19?
The symptoms of COVID-19 in children are similar to that of many childhood viral illnesses. If your child is displaying mild symptoms, it is advised to perform a home Antigen Rapid Test (ART) on them.
If the ART test result is positive but your child is otherwise well:
Visit your nearest swab-and-send-home (SASH) GP clinic to be assessed non-urgently. The list of clinics may be found at this website: https://flu.gowhere.gov.sg/.
Call ahead to check that the clinic is able to perform ARTs or polymerase chain reaction (PCR) tests for the age of your child and their operating hours for swabs.
Take your child to the clinic using private transport, taxis or private car hires with air-conditioning turned off and windows wound down to get to and from the clinic.
If the ART test result is negative but your child is unwell or displaying more severe symptoms:
Bring your child to see a doctor. Further testing with a PCR test may be required to ascertain COVID-19 or otherwise.
Following this assessment by the doctor, children who are unwell or have risk factors may be conveyed to hospital or a care facility. The majority of children would be eligible to recover from home.
Regardless of your child’s age, seek medical attention immediately at your nearest Urgent Care Centre (UCC) if he or she is displaying any of the following symptoms:
- Rapid breathing
- Breathlessness
- Poor feeding
- Drowsiness or lethargy
- High fever of more than 40 degrees
- Fever of 38 degrees or more lasting more than 5 days
- Sudden confusion
- Face or lips turning blue
- Signs of dehydration such as no urine output for more than 6 hours
- Persistent vomiting, diarrhoea or abdominal pain
Q5: How frequently should I test my child for COVID-19?
While there is no standard directive on how often your child should be tested, I would advise that if you suspect your child is displaying either COVID-19 or respiratory symptoms, they should be tested at the onset of symptoms with an ART kit.
They should also test daily before going outdoors until the symptoms fully subside upon a full recovery. It is also advisable to repeat an ART just prior to sending your child back to school.
Q6: What should I do if my child tests positive for COVID-19 and can recover from home?
Your child may recover at home if his or her test results return positive and:
- Has been assessed by a doctor to have mild or no conditions, and declared clinically suitable for home recovery
- Is above 3 months old
However, while recovering at home your child would need to adherne to the following:
- Self-isolate at home for 72 hours
- Take an ART test after 72 hours
- If he or she tests negative, they may resume their normal activities.
- If he or she tests positive, continue to have your child isolated and repeat the ART test each day. If your child tests negative during a subsequent test, they may resume their normal activities.
- If your child is fully-vaccinated or under the age of 12, they may automatically exit self-isolation from day 7, at 12pm.
- If your child is above the age of 12 and not fully-vaccinated, they may automatically exit self-isolation from day 14, at 12pm.
Should your child’s symptoms worsen during this period, do not hesitate in seeking immediate medical attention at your nearest UCC.
Q7: What kind of treatment will a child with COVID-19 receive?
If your child has COVID-19, and is recovering at home
If your child is showing mild or no symptoms, they may not need any specific treatment. While your child recovers at home, you can support their recovery in the following ways:
- Ensure that your child has adequate rest and drinks lots of fluids.
- You can give your child medication to relieve their symptoms of fever, nasal congestion, runny nose or cough to keep them comfortable.
- Keep your child in a room separate from other household members, and away from communal areas of the house since the virus is spread via droplets and contact. This will also help protect vulnerable elderly living in the home from being infected.
- Avoid switching on the air-conditioner for your child in the isolation room and open the windows of the room to keep it well-ventilated.
- Monitor your child’s temperature, pulse, and oxygen saturation (unless they are very young, then the pulse oximeter might not fit on your child’s fingers) and other symptoms closely.
- Seek a telemedicine consultation if your child’s condition doesn’t improve.
If your child develops more serious symptoms
If your child develops more severe symptoms from COVID-19 or MIS-C, they would need urgent hospital care. They might need oxygen supplementation or intravenous fluids to support their recovery. Seek medical attention immediately.
Q8: Will I be allowed to stay with my child if he or she needs isolation for COVID-19?
Most hospitals are adopting a single accompanying parent policy for all unwell children who are admitted to hospital. If your child is isolated for suspected COVID-19, one parent is allowed to accompany the child.
Since your child will be isolated, you will need to remain in the isolation facility throughout your child’s stay as well. If your child tests positive for COVID-19, you will be placed under quarantine and closely monitored for the development of any respiratory symptoms.
Q9. How can I step up my efforts to protect my child from catching COVID-19, especially from school?
Vaccination
According to the Ministry of Health (MOH) Singapore, vaccinating your child is advised to reduce the chances of them contracting COVID-19 and developing severe disease. Vaccination also protects children from transmitting the virus to others and keeps their family members and school mates safe. At present, Singapore has rolled out vaccination efforts for children aged 5 years old and above.
Good hygiene practices
Imparting good hygiene practices is paramount in keeping the virus at bay. Encourage your family, including your child, to incorporate these practices into their daily routine:
- Wash hands with soap and water thoroughly and regularly for at least 20 – 30 seconds, or use an alcohol-based hand sanitiser containing at least 60% alcohol and rub it with their hands for 20 seconds.
- Sneeze into a tissue, away from others or into your elbow to limit the spread of germs.
- Wear a face mask if your child is above 3 years old. Ensure that the mask covers your child’s nose and that they handle the placing and removal of the mask with clean hands. They should not touch the exterior surface of the mask.
- If your child is 6 years old and above, he or she is required to wear a face mask as mandated by MOH.
- If your child is under the age of 6 but above the age of 3, encourage him or her to wear a face mask or face shield especially if they are in a group setting or interacting with others, provided they can handle a mask safely without supervision.
- If your child is under the age of 3, wearing a face mask is not recommended.
- Practice safe distancing outside of your immediate family.
Q10: Is COVID-19 vaccination safe for children between 5 – 11 years old?
The Health Sciences Authority (HSA) has endorsed the safety, efficacy and quality of the Pfizer-BioNTech/Comirnaty COVID-19 vaccines on children 5 years and above. The HSA and Expert Community on COVID-19 Vaccination (EC19V) have also reported that in totality, the benefits of the Pfizer-BioNTech/Comirnaty vaccine outweigh the risks when used in a paediatric dosage (10 micrograms) for children aged 5 – 11 years, which is a third of the dosage given to children aged 12 and above. Clinical trials also show a 90% reduction in the risk of symptomatic infection in infected children.
What are the side effects of COVID-19 vaccination in children?
Side effects are mild to moderate, and tend to resolve in a few days. Your child may experience more side effects after the second shot, which is a sign that their body is building defences against the virus. Serious adverse effects are rare. However, if you notice that your child has any of the following symptoms, seek medical attention immediately:
- A fever that persists for more than 48 hours
- Respiratory symptoms such as cough, runny nose, sore throat, shortness of breath or loss of sense of taste and smell
- Chest pain, shortness of breath or abnormal heartbeat
- A side effect that is prolonged, or gets worse
- An allergic reaction such as rash, hives, swelling, breathlessness or fainting
Q11: Can I breastfeed my child if either one of us contracts COVID-19?
Based on experience with other respiratory viruses, the transmission of viruses via breast milk is likely to be less significant in comparison to the benefits of breastfeeding.
However, if you have been diagnosed with COVID-19, you should take extra precautions to prevent transmission of the virus to infants through respiratory droplets and contact. This would include wearing a face mask when breastfeeding and taking strict hand hygiene measures when handling your baby. Take adequate hygiene precautions when handling expressed milk as well.
If your child is diagnosed with COVID-19, you can continue breastfeeding. Wear a mask to protect yourself and practise good hand hygiene. You should seek medical attention early if you develop fever or any respiratory symptoms.
Q12: Should I avoid going to hospitals with my child or delay hospital follow-ups for vaccinations or my child’s chronic illnesses?
It is important to continue routine vaccinations for your child and regular follow-ups to monitor your child’s chronic medical conditions. You can postpone other non-urgent medical consults.
Some paediatric clinics provide time slots in the mornings only for routine health assessments (for growth and development) and vaccinations. It is recommended that advanced appointments be made so clinic staff can make the necessary arrangements. Routine vaccinations will protect your child from acquiring childhood diseases such as measles, diphtheria, Haemophilus influenzae, pneumococcal pneumonia, all of which have much higher mortality rates in children than COVID-19.
If you have respiratory symptoms (eg. cough, runny nose or fever), please visit your nearest Public Health Preparedness Clinic. It is important to receive timely treatment for your condition.
Child Vaccination. Ministry of Health Singapore. Retrieved 25 January 2022 from https://www.moh.gov.sg/covid-19/vaccination/faqs---children-related-vaccination-matters
What Happens When Kids Get Long-COVID? Yale Medicine. Retrieved 2 November 2021 from https://www.yalemedicine.org/news/long-covid-in-kids
Everything you need to know about washing your hands to protect against coronavirus (COVID-19). Unicef. Retrieved 5 October 2021 from https://www.unicef.org/coronavirus/everything-you-need-know-about-washing-your-hands-protect-against-coronavirus-covid-19
FAQs – Masks and Personal Protective Equipment (PPE). Ministry of Health Singapore. Retrieved 9 July 2021 from https://www.moh.gov.sg/covid-19/general/faqs---masks-and-personal-protective-equipment-(ppe)
Children & COVID-19. World Health Organization. Retrieved 21 January 2021 from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/media-resources/science-in-5/episode-22---children-covid-19
Covid-19 Home Recovery Survival Guide: How to disinfect your room and other precautions. The Straits Times. Retrieved 20 October 2021 from https://www.straitstimes.com/life/covid-19-home-recovery-survival-guide-how-to-disinfect-your-room-and-other-precautions
Coronavirus (COVID-19): What to Do if Your Child Is Sick. Nemours KidsHealth. Retrieved 5 January 2022 from https://kidshealth.org/en/parents/coronavirus-child-is-sick.html
Well and Test Positive, or Condition Assessed Mild by Doctor. Ministry of Health Singapore. Retrieved 5 January 2022 from https://www.covid.gov.sg/well-and-positive-or-condition-assessed-mild-by-doctor
What to do if you or your child gets sick with COVID-19 at home. Unicef. Retrieved 18 January 2022 from https://www.unicef.org/coronavirus/caring-for-sick-person-covid-home
COVID-19 vaccination for children aged 5-11 years old. Ministry of Health Singapore. Retrieved January 2022 from https://www.moh.gov.sg/docs/librariesprovider5/vaccination-matter/child-vax_brochure_v2_2jan-(2-edits).pdf
COVID-19 in Babies and Children. May Clinic. Retrieved 28 January 2022 from https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-in-babies-and-children/art-20484405
Woodruff, R; Campbell, A.P; Taylor, C.A, et al. (2021, December 22), Risk factors for severe COVID-19 in children. American Academy of Pediatrics, 149 (1). https://publications.aap.org/pediatrics/article-abstract/149/1/e2021053418/183463/Risk-Factors-for-Severe-COVID-19-in-Children?redirectedFrom=fulltext
Buonsenso, D; Munblit, D; De Rose, C; et al; (2021, July), Preliminary Evidence on long COVID in Children (2021, April 7), Acta Paediatrica, 110 (7). doi: 10.1111/apa.15870
Sperotto, F; Friedman, K.G; Son, M.B.F; VanderPluym, C.J; Newburger, J. W; Dionne, A. (2020, August 15). Cardiac manifestations in SARS-CoV-2-associated multisystem inflammatory syndrome in children: a comprehensive review and proposed clinical approach. European Journal of Pediatrics. 180(2): 307–322. doi: 10.1007/s00431-020-03766-6
What Happens When Kids Get Long-COVID? Yale Medicine. Retrieved 2 November 2021 from https://www.yalemedicine.org/news/long-covid-in-kids
Everything you need to know about washing your hands to protect against coronavirus (COVID-19). Unicef. Retrieved 5 October 2021 from https://www.unicef.org/coronavirus/everything-you-need-know-about-washing-your-hands-protect-against-coronavirus-covid-19
FAQs – Masks and Personal Protective Equipment (PPE). Ministry of Health Singapore. Retrieved 9 July 2021 from https://www.moh.gov.sg/covid-19/general/faqs---masks-and-personal-protective-equipment-(ppe)
Children & COVID-19. World Health Organization. Retrieved 21 January 2021 from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/media-resources/science-in-5/episode-22---children-covid-19
Covid-19 Home Recovery Survival Guide: How to disinfect your room and other precautions. The Straits Times. Retrieved 20 October 2021 from https://www.straitstimes.com/life/covid-19-home-recovery-survival-guide-how-to-disinfect-your-room-and-other-precautions
Coronavirus (COVID-19): What to Do if Your Child Is Sick. Nemours KidsHealth. Retrieved 5 January 2022 from https://kidshealth.org/en/parents/coronavirus-child-is-sick.html
Well and Test Positive, or Condition Assessed Mild by Doctor. Ministry of Health Singapore. Retrieved 5 January 2022 from https://www.covid.gov.sg/well-and-positive-or-condition-assessed-mild-by-doctor
What to do if you or your child gets sick with COVID-19 at home. Unicef. Retrieved 18 January 2022 from https://www.unicef.org/coronavirus/caring-for-sick-person-covid-home
COVID-19 vaccination for children aged 5-11 years old. Ministry of Health Singapore. Retrieved January 2022 from https://www.moh.gov.sg/docs/librariesprovider5/vaccination-matter/child-vax_brochure_v2_2jan-(2-edits).pdf
COVID-19 in Babies and Children. May Clinic. Retrieved 28 January 2022 from https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-in-babies-and-children/art-20484405
Woodruff, R; Campbell, A.P; Taylor, C.A, et al. (2021, December 22), Risk factors for severe COVID-19 in children. American Academy of Pediatrics, 149 (1). https://publications.aap.org/pediatrics/article-abstract/149/1/e2021053418/183463/Risk-Factors-for-Severe-COVID-19-in-Children?redirectedFrom=fulltext
Buonsenso, D; Munblit, D; De Rose, C; et al; (2021, July), Preliminary Evidence on long COVID in Children (2021, April 7), Acta Paediatrica, 110 (7). doi: 10.1111/apa.15870
Sperotto, F; Friedman, K.G; Son, M.B.F; VanderPluym, C.J; Newburger, J. W; Dionne, A. (2020, August 15). Cardiac manifestations in SARS-CoV-2-associated multisystem inflammatory syndrome in children: a comprehensive review and proposed clinical approach. European Journal of Pediatrics. 180(2): 307–322. doi: 10.1007/s00431-020-03766-6