-
-
Featured Care Areas


Source: Shutterstock
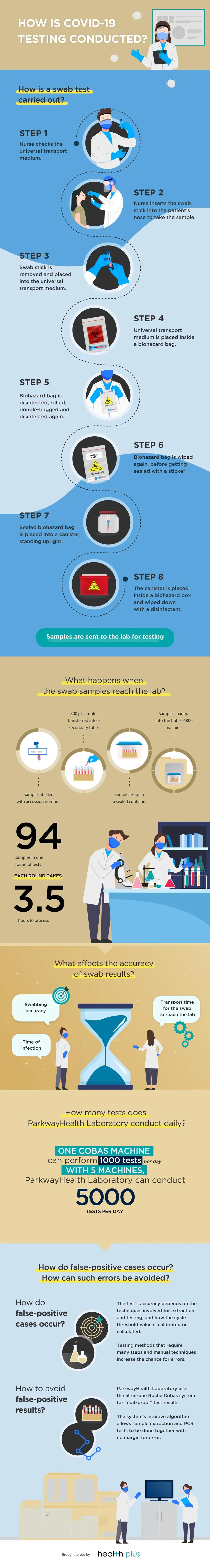
How is COVID-19 Testing Done?
Last updated: Monday, November 2, 2020 | 4 min reading time
How do you get tested for COVID-19?
There are currently 2 ways to test for COVID-19 – a diagnostic test and an antibody test. In a diagnostic test, samples of cells and fluids from the nose or throat are often collected using a nasal swab, before the samples are processed by a machine which detects the virus’s genetic material. An antibody test, also known as a serology test, is conducted using a blood sample to detect evidence of the body’s immune response to the virus after an infection.
ParkwayHealth Laboratory conducts diagnostic tests, also known as molecular polymerase chain reaction (PCR) tests, using the cobas® 6800 System (a molecular test system developed by Roche). Each day, up to 5,000 of these tests, known technically as COVID-19 SARS-CoV-2 PCR tests, are carried out at the ParkwayHealth Laboratory facilities. In a Channel News Asia feature, ParkwayHealth Laboratory shares what happens behind the scenes from sample collection to laboratory testing.
How is a nasal swab test carried out?
First, the nurse checks that the universal transport medium is in good condition and has not expired. The transport medium is used to preserve the sample and maintain its original state.
The patient is then advised to clear their nose. Next, the patient tilts their head upwards, and the nurse inserts the swab stick into the patient’s nose to obtain a sample. The swab stick is removed and placed into the universal transport medium.
For safety, this is then placed inside a biohazard bag, and wiped down with a disinfectant (MICRO-CHEM PLUS detergent disinfectant cleaner, or ethanol) and then rolled up. As an additional safety measure, the sample is double-bagged and disinfected again before being sealed with a sticker.
The sealed biohazard bag is then placed into a canister, standing upright. The canister is placed inside a biohazard box and wiped down with a disinfectant before finally being sent to the laboratory for testing.
What happens when the swab samples reach the lab?
Once the samples reach the lab, the technician will label each sample with a laboratory-generated accession number, which is a unique identification number. 800μl of the sample is transferred into a secondary tube. The sample transfer is carried out carefully, and care is taken to prevent cross-contamination. These samples will be kept in a sealed container and carried to the testing machine. Finally, the samples are loaded into the cobas® 6800 machine. The test can pick up to 94 samples in one batch, with each batch taking approximately 3.5 hours to process.
What affects the accuracy of swab results?
The accuracy of swab results depends a lot on the way the swabbing is carried out to obtain the test sample. Time taken for the swab to reach the lab is also an important factor as the sample may degrade over time, especially in hot weather. Time of infection may also affect the accuracy of the swab results – if the swab is taken too early or too late, the test may give a false-negative result.
How many tests does ParkwayHealth Laboratory conduct daily?
One cobas® 6800 machine can perform 1, 000 tests per day. With 5 machines, Parkway Laboratory Services can conduct 5,000 tests per day.
How do false-positive cases occur? How can such errors be avoided?
The accuracy of the test result often depends on the techniques involved for extraction and testing, and how the cycle threshold value (cut-off point to determine a positive or negative result) is calibrated or calculated. Some testing methods require many steps and manual techniques, including pipetting, calibrating and calculating the cycle threshold value – this increases the chance for errors. ParkwayHealth Laboratory uses the Roche cobas® system, which is a closed or all in one system, with the machine doing both the extraction and PCR test to obtain an “edit proof” test result. The Roche cobas® system uses an intuitive algorithm within the testing machine because it does the extraction and PCR, both all in one.
How does Parkway Laboratory Services cope with the shortage of test kits?
Diversifying supplies is essential to cope with the shortage of test kits and important in building testing resilience for the whole community. Due to the global rise in testing, many suppliers of test kits and reagents are unable to keep up with the demand. A well-known example is Qiagen’s extraction kit, which is suffering a global shortage because of an overwhelming global demand.
ParkwayHealth Laboratory has also collaborated with local research agencies like A-star and DSO laboratories, and this partnership has helped them ramp up the local production of PCR test kits. Apart from local agencies, ParkwayHealth Laboratory also relies on Roche and other major vendors like Qiagen for testing components.
Will mass testing become part of daily life?
Until the vaccines are approved, mass testing will be the only weapon to prepare for future COVID-19 infections. Testing is the only strategy that can quickly identify COVID-19 infected individuals, isolate them and break the transmission – mass testing can help investigators isolate populations in a more refined manner. Experts suggest that testing should be integrated with precautions like social distancing, hand washing and face masks.
PCR tests are now available to all individuals who require them. Visit Parkway Shenton clinics or call +65 6227 7777 for more information.
Coronavirus Testing Basics. Retrieved 5 October 2020 from https://www.fda.gov/consumers/consumer-updates/coronavirus-testing-basics